The field of medical respite care continues to grow and evolve as communities across the U.S. increasingly recognize the value of providing people experiencing homelessness a place to recuperate from surgery or illness when they don’t require hospitalization.
NIMRC was established in 2020 by the National Health Care for the Homeless Council to help meet this rapidly growing critical need. NIMRC advances best practices, delivers expert consulting services, and disseminates state-of-field knowledge in medical respite care.
The NIMRC team also collects and shares data from medical respite programs so we can provide a snapshot of programs nationwide.
Here are five things we know, based on the data, about the state of medical respite care in 2023:
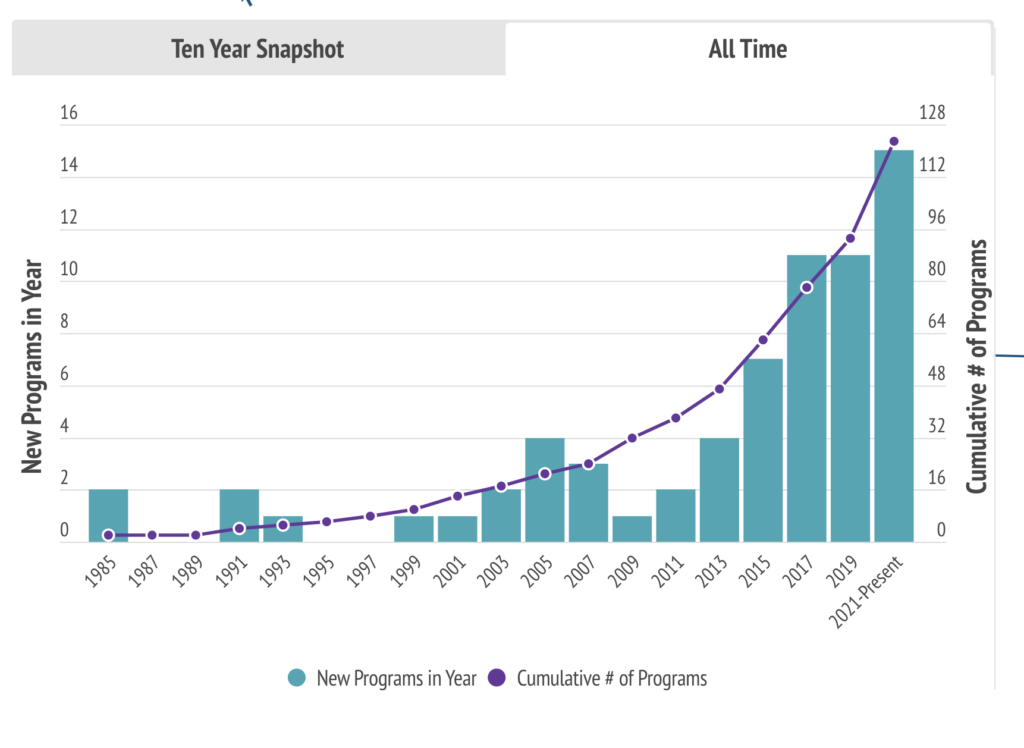
1. The need for medical respite care is expanding faster than ever
Housing is an essential part of health care, and recovering from acute health conditions is often not possible for people living outside or on the streets. The COVID-19 pandemic illuminated the challenges our hospital and health care systems have with meeting the needs of our communities. Not only are there more people experiencing homelessness than ever in the US, there are more elders with complex and serious health conditions living on the streets. MRC programs fill an immediate gap and improve individual health and community health equity. This brief intervention can change a person’s life trajectory and alleviate hospital systems, allowing them to provide more quality care to communities at large.
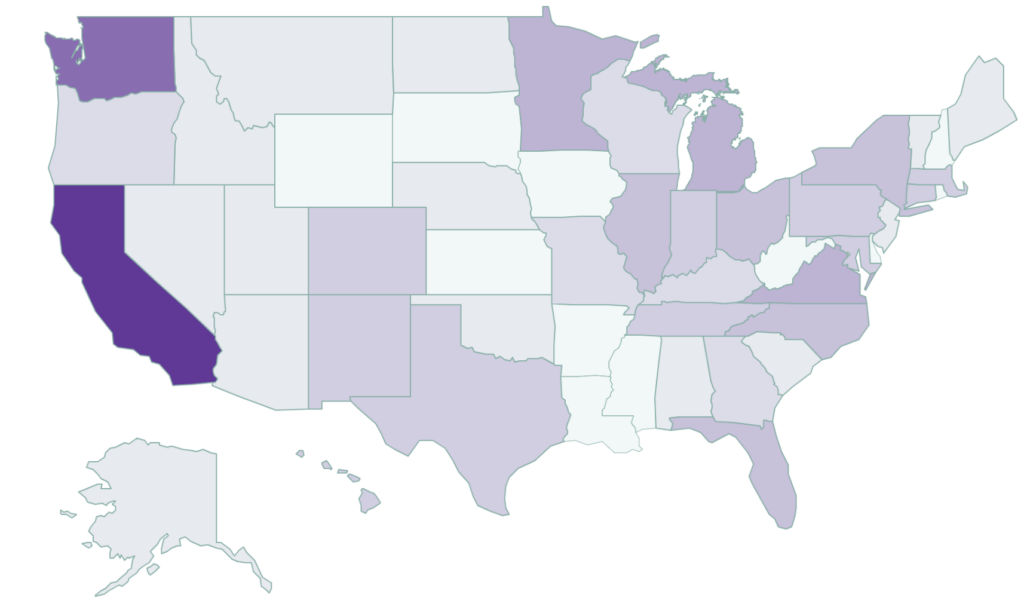
2. California is leading the way
California not only has the highest number of facilities offering medical respite services (45+), the state also is leading the way on incorporating medical respite care into the services Medicaid will pay for, helping us to collaboratively form blueprints and action plans that will help other states follow suit to meet their unhoused residents’ needs.
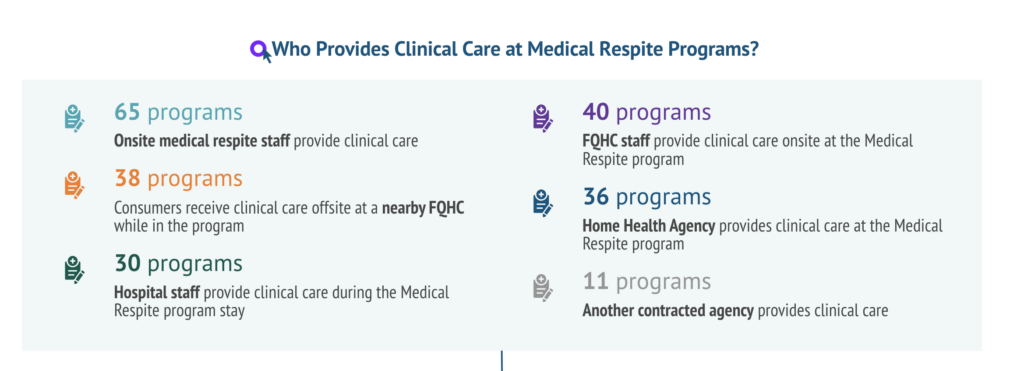
3. The needs of medical respite care patients are unique and complex
Nearly half of the programs included in our reporting say they utilize multiple sources for clinical care for their patients. Medical respite programs provide care in a wide range of ways and often form partnerships with other organizations to meet the complex needs of their consumers. Behavioral health care is emerging as an immediate need that many MRC programs are supporting. As the field emerges, conversations about strategies to support all acute health needs (physical and mental) are being integrated into the field.
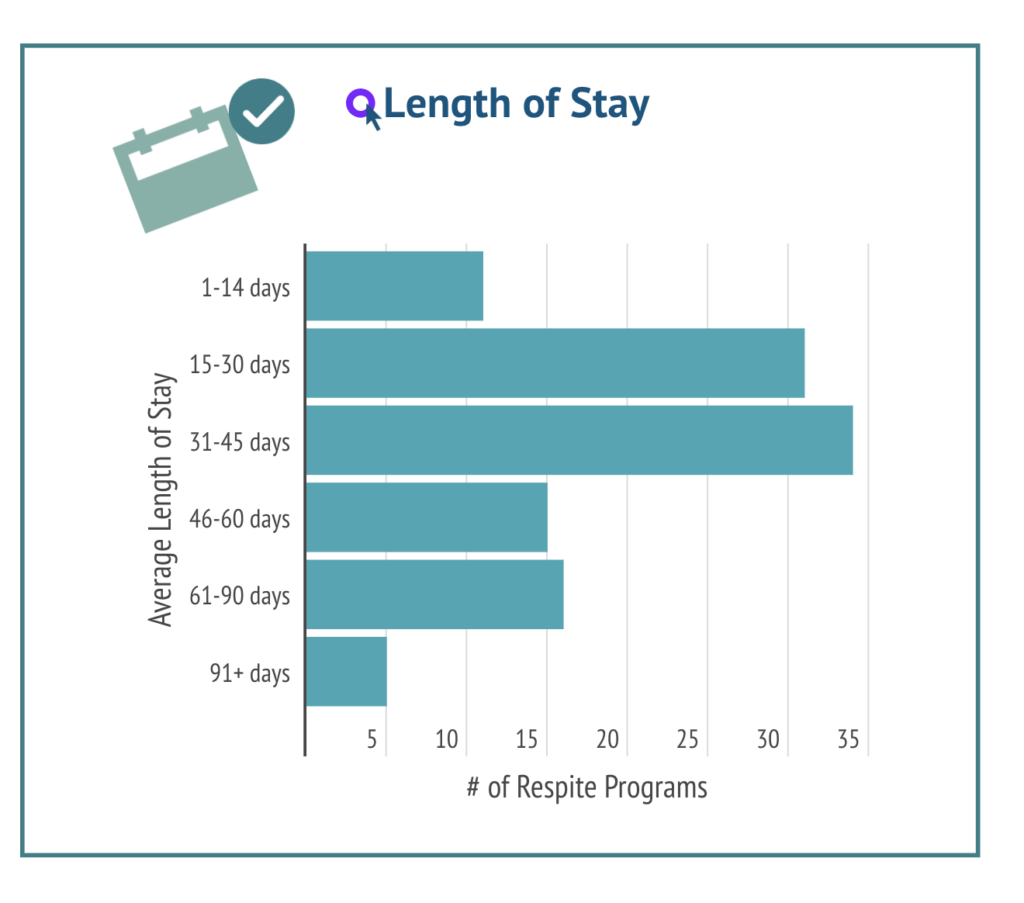
4. The average medical respite patient stay is between 31 and 45 days
Recovering from illness or surgery is difficult when you’re experiencing homelessness. Having a safe, clean space to rest and recover for as long as is needed is a human need and a human right. Various studies have shown longer lengths of hospital inpatient stays and higher readmission rates for people experiencing homelessness. One study found that people experiencing homelessness average a 30-day emergency department (ED) readmission rate 5.7 times higher and a hospital inpatient rate 1.9 times higher than their housed counterparts. Having access to medical respite services can reduce lengths of stay in hospitals as well as contribute to better overall outcomes. For example, in Boston, patients who had access to medical respite care had a 50% reduction in the odds of readmission at 90 days post discharge. (Source)

5. Peer support programming is an important part of medical respite care
There are several emerging practices and services in medical respite programs around the country, but perhaps the most popular emerging practice is having peer support available through individuals who have life experiences in common with medical respite care consumers. People with shared lived expertise have a unique capacity to help based on a shared affiliation and a deep understanding of particular experiences.
To learn more about establishing a medical respite care program in your community, reach out to our team!
The data above is self-reported by MRC programs based on their profile submissions in the Medical Respite Program Directory. If your MRC program is not represented here or if you would like to provide updated information, please complete this program profile form. Our team periodically updates these figures as new data emerges!


